Definition:
Ankylosing Spondylitis is a chronic inflammatory condition of the spine and sacro-iliac joints characterised by osseous proliferation and the development of a progressive kyphotic spinal deformity in the most severe classical cases.
Incidence:
The disease affects approximately 1 per every 1,000 people with a lower incidence in black Americans.
Classic Ankylosing Spondylitis affects males more commonly than females, but the overall incidence is similar and symptoms usually develop between 15 – 25 years of age.
Clinical Features:
The onset is usually insidious with the development of back-ache and stiffness.
In women the diagnosis may be delayed but progressive disease is less common and there is usually more peripheral joint, and less spinal involvement.
In the classical form there is loss of spinal mobility (extension first) with flattening of lumbar lordosis.
Ocular inflammation occurs in about 1/3 of patients (uveitis in about 20% and conjunctivitis in 25%).
Active inflammatory disease may be associated with weight loss, fatigue and a low grade fever.
Treatment:
Anti-inflammatory medication, analgesics and physiotherapy help to relieve symptoms and maintain movement.
Rest and immobilisation is contraindicated as this tends to increased osteoporosis, deformity and the restriction of joint and spinal movement.
Where spinal deformity is severe, restricting function and mobility, a spinal osteotomy (lumbar or cervical) may become indicated to improve the patients “outlook on life”.
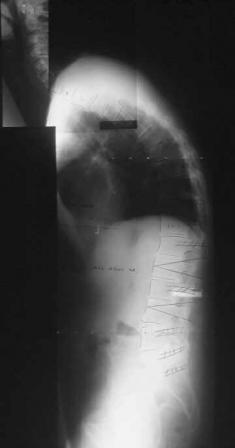



The images above display the pre-operative radiograph and clinical photograph of a patient with Ankylosing Spondylitis. The post-operative x-ray and clinical photograph is also shown for comparison.
A spinal osteotomy is however a major operation with associated significant risks, and is only indicated when deformity is severe and associated with significant disability.
Prognosis:
The age of the individual at the onset of symptoms is the most important factor in determining the prognosis and outcome.
